Hi, my name is Allison Schaaf, my own fertility journey, including 5 miscarriages, inspired me to create this website to help YOU navigate your own fertility journey.
Here are my main takeaways I would share with you as a friend:
- Uterine septum is a structural issue that can cause miscarriage
- There is testing you can do to determine if you have a uterine septum
- If you do have uterine septum, there are procedures to remove the septum and improve chances of a healthy pregnancy
Of course, I also recommend you work with your doctor and do your own research! I have coordinated these articles with the nitty-gritty details and links to research so you can decide what works best for you, read on for more. And don’t miss my Action Steps at the bottom of the article!
Table of Contents
What is uterine septum?
Symptoms of uterine septum
How uterine septum affects pregnancy
Why uterine septum causes miscarriage
Diagnosis of uterine septum
Treatments for Uterine Septum
Uterine septum is the most common form of uterine deformity. Up to 10% of women with three or more consecutive recurrent miscarriages have uterine septum. These miscarriages tend to be within the first or second trimester. Fortunately, it is treatable, and up to 86% of women with uterine septum can have successful pregnancies. 1 This article will provide you with everything you need to know about uterine septum.
What is uterine septum?
A uterine septum or septum uteri (in Latin) is a form of a congenital uterine malformation found in 0.1 – 1.5% of women. 3 A normal uterine cavity is a narrow and empty space. But when the septum is present, it longitudinally partitions the uterine lumen, although the outer form of uterus remains in its pear-shaped form. 4
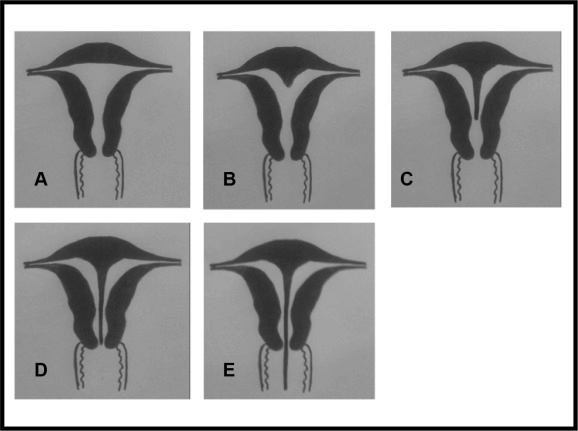
There are two different types of uterine septum based on the septum distribution: 5
- Incomplete septum – the partial septum in the top portion of the uterus
- Complete septum – the septum spans the total height of the uterine cavity. The septum may also extend into the cervix or vagina (see images C – E above).
Symptoms of uterine septum
There is no symptom associated with having a uterine septum. You may be completely unaware of it until you try for a baby. Many women only discover it as they investigate fertility issues, recurrent miscarriages, or through a uterine ultrasound examination. 6
How uterine septum affects pregnancy
Many women with uterine septum have normal and uneventful pregnancies and reproductive function. 7 However, a longitudinal study involving 3181 women reported a 26% incidence of first-trimester spontaneous miscarriage and a 6% incidence of second-trimester miscarriage. 8 Whereas, some other studies reported up to a 65% spontaneous miscarriage rate among women with uterine septum. 9 If you have repeated miscarriage during the 2nd trimester with obvious signs of labor, your doctor might suspect a uterine septum. 10
The uterine septum may contribute to other poor pregnancy outcomes, including malpresentation, preterm delivery, intrauterine growth restriction, placental abruption, and overall perinatal mortality. 11
Many women with uterine septum experience breech presentations (25%–30%), oblique and transverse positions (5%), and premature labor (20%) in their pregnancies. About 5 – 10% of these women retain the placenta in their uterus after delivery. 12
Why uterine septum causes miscarriage
The following are some possible theories that explain why recurrent abortions occur in women with septum uteri.
1) Endometrial dysfunction and decreased luminal (hollow) space
The endometrium is the inner lining of the uterus, which accepts the embryo and forms the placenta with embryonal tissue. The septum, unlike the uterine lining, may not develop fully for implantation. 13 If the fertilized embryo settles into the septum or the disrupted endometrial tissue, it may fail to implant properly and result in a miscarriage. 1415
2) Increase in fibromuscular tissue, allowing the cervix to dilate
The uterine septum can reduce the uterine muscle’s resistance to cervical dilation, causing miscarriage. 16
3) Poor blood vessel nourishment in the septum
The fetus depends on the blood vessels in the endometrium for nourishments like nutrients and oxygen. The septum may have fewer blood vessels (vascularization) than what the fetus needs. This can restrict fetal growth or lead to a miscarriage. 17
Diagnosis of uterine septum
Because septum uteri typically don’t cause any symptoms, your doctor may only diagnose and treat it on the basis of reproductive problems. Sonohysterography (SHG) is the method of choice for diagnosing uterine septum. In cases of contraindications, such as contrast dye allergy or pelvic inflammatory diseases, your doctor may opt for hysteroscopy or laparoscopy instead.
As part of your routine health checks, your doctor may first perform a pelvic examination to exam the vulva and your reproductive organs. In most patients, the finding is completely normal unless the septum extends into the cervix or vagina.
Uterine septum is typically diagnosed with transabdominal and transvaginal ultrasound, especially with 3D advanced machines (3D ultrasound). 18
Transabdominal ultrasound is performed across the belly. To prepare for this exam, avoid eating to eat 4-5 hours beforehand and drink a lot of water for better visualization (3-4 glasses of water every half an hour). Your doctor will put the gel on the probe and scan your belly. The examination lasts a few minutes.
Transvaginal ultrasound is performed through your vagina. You should empty your bladder before the examination. Your doctor will put a condom on the probe and the gel over it. You may feel some discomfort as the probe enters the vagina. This exam is also short, lasting only a few minutes.
Sonohysterography (SHG) is a special type of transvaginal uterine ultrasound where your doctor injects a contrast dye into the uterus to better see the septum inside the uterus. 19
For this procedure, your doctor will first examine the uterus just with a transvaginal ultrasound before injecting a contrast dye into the uterine cavity with a speculum. Then, they will insert the transvaginal probe to perform an exam.
The SHG usually takes around half an hour. You should empty your bladder beforehand. Your doctor may recommend some over the counter painkiller to reduce your discomfort or cramping following the procedure. Contraindications for SHG include pregnancy and pelvic inflammatory disease, so they will exclude this at first examination. The optimal timing for an SHG is right after menstrual bleeding.
Light bleeding over the next few days after the procedure is normal, and you shouldn’t be alarmed if it is only a few drops.
Note: Although easily confused due to similar names, SHG is not the same test as hysterosalpingography (HSG). An HSG is an X-ray scan to show the shape of the uterus and see whether the fallopian tubes are blocked. The SHG is an ultrasound-based examination.
A hysteroscopy involves examining the internal structures of the uterus using a hysteroscope, inserted into the uterus through the vagina. A hysteroscope is a narrow telescope with a light and camera at the end. 2021
In some cases, it is tricky to diagnose a uterine septum correctly because it can be confused with a bicornuate (heart-shaped) uterus. Many OB/GYNs use 3D ultrasound combined with sonohysterography. While the HSG test can screen for uterine malformations, it often cannot reliably distinguish between a septated uterus and a heart-shaped one. So, when all other methods fail to tell apart these two possibilities, your doctor may recommend a laparoscopy (keyhole surgery) to clearly see the uterus and septum. 22
Treatments for Uterine Septum
It is entirely possible to conceive normally and maintain a healthy pregnancy even with uterine abnormalities. In fact, the majority (75%) of women with congenital uterine malformations have normal reproductive function. 23
If the uterine septum does not cause pregnancy or fertility problems, the risk for surgical intervention may exceed the benefit. Each doctor may have their own opinion on whether to remove a septum preventatively or as an infertility treatment. Since infertility seldom results from a uterine anomaly alone, the mere diagnosis of septum uteri does not warrant a surgery. 24
If you have had multiple miscarriages, pregnancy complications, or infertility issues caused by the septum, your doctor may recommend surgery to remove the septum (metroplasty).
Hysteroscopic metroplasty surgery for uterine septum
Clinical studies have shown that hysteroscopic septum incision reduces miscarriage rates and improves live-birth rates in patients with a history of recurrent pregnancy loss. 25262728
Hysteroscopic removal of a uterine septum is the preferred method of septum removal. During this procedure, your gynecologist cuts out the septum while visualizing it with a hysteroscope. It is an outpatient and minimally-invasive procedure as there is no abdominal incision.
Preparing for a hysteroscopic septum removal – Although the surgery is minimally invasive, it requires general anesthesia, so you may be advised to avoid eating for at least 6 hours before the procedure. 29 The procedure can last from half an hour to around 2 hours. You should also avoid vaginal sex one day before the procedure. Vaginal medications or tampons should also be avoided 24h prior to the procedure. If you have any allergies or take blood-thinning drugs, you should inform your doctor. Contraindications for this procedure include pregnancy and sexually transmitted diseases, so your doctor should exclude or treat any STDs beforehand. The optimal timing for the procedure is in the first half of the cycle and right after bleeding.
After the surgery, you may feel slight vaginal pain and have light vaginal bleeding up to a week post. Avoid sex, tampons, and heavy physical activities for at least a week. If you start feeling feverish, abdominal pain, abundant vaginal bleeding, or smelly secretion, contact your OB/GYN immediately.
Like every procedure with general anesthesia, the risks may include nausea, vomiting, after procedure pain, throat soreness, respiratory failure, cardiac failure, allergic reaction, and death (rarely). Complications of this procedure are rare but may include bleeding, infection, uterus perforation, air embolism, and pulmonary embolism. 30 Also, remember to notify your doctor and share your medical history, especially if you have diabetes or take blood thinners such as aspirin, heparin, or warfarin. 31
Following-up after a hysteroscopy, your doctor may perform an ultrasound scan and a pelvic examination about one menstrual cycle after the surgery to ensure that the uterus is completely healed. Once the uterus heals, there should not be any scarring, abnormal granulation, or bleeding.
When should you try again after a uterine septum surgery?
After a metroplasty, you should wait for at least two menstruations before trying for pregnancy again during the third ovulation. One study investigated 16 patients after this surgery and found that 19% of patients fully healed by 1 month and 100% of patients fully healed by 2 months. 32
Another retrospective study explored pregnancy rates in 282 women after IVF/ICSI when the embryo transfer was performed at<9, 10–16, or>17 weeks following uterine septum incision. Pregnancy rates and miscarriage rates were the same among the three groups. 33
Conclusion
Approximately 1.5% of all women, and up to 10% of those with recurrent pregnancy loss have uterine septum. It may contribute to first or second trimester miscarriages, or other pregnancy complications such as breech presentation and intrauterine growth restriction. For many women with septate uterus and recurrent miscarriages, surgical removal of uterine septum reduces miscarriage rates and improves live birth rates. If you suspect you may have a uterine septum, speak to your doctor about getting a sonohysterography (SHG) or hysteroscopy examination.
Next Steps to Consider
- If you have experienced a miscarriage or unexplained fertility issues, ask your doctor about having a hysterocopy to rule out uterine septum
- If you have a uterine septum, consider surgery to remove and increase your chances of a healthy pregnancy
References




0 Comments