Hi, my name is Allison Schaaf, my own fertility journey, including 5 miscarriages, inspired me to create this website to help YOU navigate your own fertility journey.
Here are my main takeaways I would share with you as a friend:
- Thyroid issues are a common contributor to infertility and miscarriage, this article takes an in-depth look at testing for thyroid levels.
- Thyroid levels can change over time, including after a pregnancy or miscarriage, so it is important to re-test levels on a regular basis.
- Women with thyroid issues can have this condition under control and maintain healthy pregnancies.
Of course, I also recommend you do your own research! That is why I have coordinated these articles with the nitty-gritty details and links to research so you can best decide what works best for you, read on for more! And don’t miss my Action Steps at the bottom of the article!
Table of Contents
Introduction: the thyroid gland and axis
Thyroid examination and tests for miscarriage
How thyroid hormones fluctuate during pregnancy
Thyroid disorders affect many women, and undiagnosed thyroid disorders are surprisingly common. You may not be aware of your thyroid disorders, especially stealth ones, which can cause infertility and miscarriages. Up to 15% of reproductive age women have thyroid antibodies, many of which have perfectly normal thyroid function 1.
About 17 – 33% of women with recurrent miscarriages have thyroid antibodies 23. Also, sometimes, pregnancy or previous miscarriage can trigger a thyroid condition or antibodies. This article, part 1 of a 2-part series, will introduce you to:
- The thyroid axis, which includes a collection of factors influencing thyroid functions
- Thyroid tests to keep track of to rule out hypothyroidism, hyperthyroidism, and thyroid antibodies as a cause of miscarriage.
To learn more about thyroid conditions, including symptoms, diagnosis criteria, and how they affect pregnancy, read part 2 of this 2-part series.
Introduction: the thyroid gland and axis
The thyroid is a butterfly-shaped gland located in the front of your neck. It secretes thyroid hormones, which controls metabolism throughout your body.
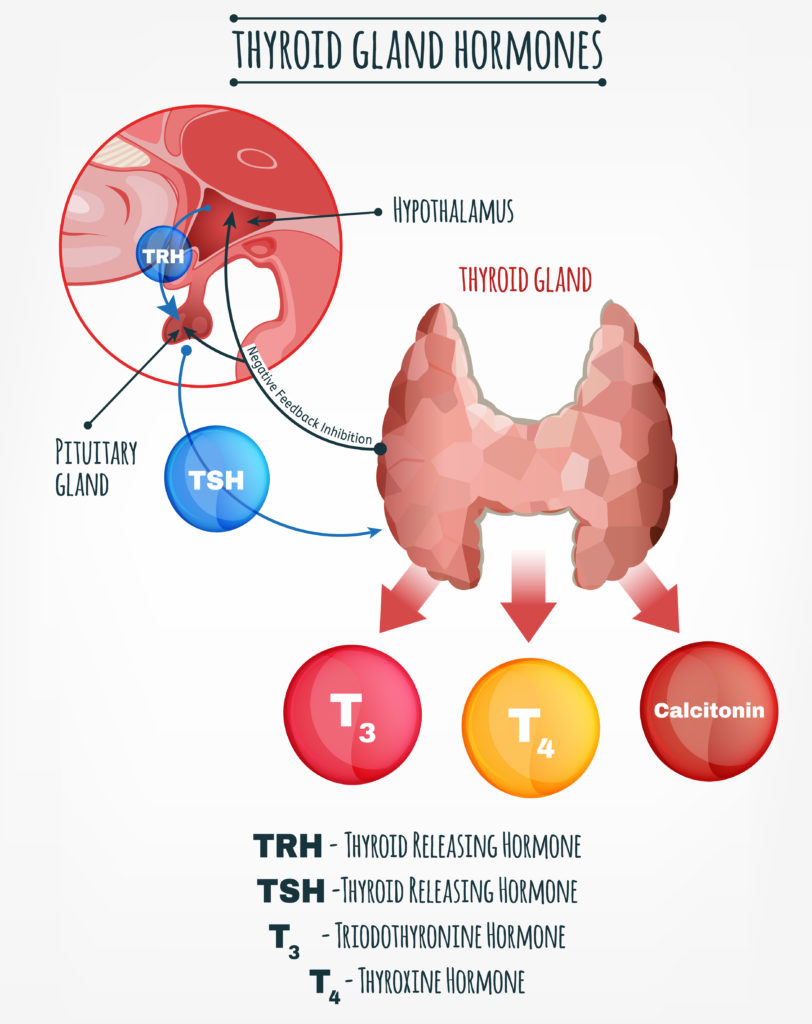
The thyroid axis includes the hypothalamus, the pituitary, and the thyroid glands. The hypothalamus and pituitary also secrete hormones that control the ovaries in women and the testicles in men, as well as adrenals.
Inside your thyroid axis, the hypothalamus secretes thyrotropin-releasing hormone (TRH), which commands the pituitary to secrete thyroid-stimulating hormone (TSH, also called thyrotropin).
TSH stimulates the thyroid to release thyroxine (T4 for having 4 iodides). T4 is the inactive “storage” thyroid hormone, which needs to be converted into T3, the active form, in order to increase energy in target cells.
The conversion into triiodothyronine (T3 for having 3 iodides) happens in target tissues, mostly in the liver but also in the gut, nerves, and placenta. Both T3 and T4 are usually referred to as “thyroid hormones.” In the bloodstream, over 99.9% of T3 and T4 bind to proteins as they travel to target organs, so less than 0.1% is free and functional 4.
Your thyroid axis has a negative feedback system similar to a thermostat to ensure you have just enough active thyroid hormones. When you have enough T3 and T4, they tell the pituitary to stop producing more TRH and TSH. This is why your doctor tests for high TSH or low TSH to screen for hypothyroidism or hyperthyroidism, respectively. However, it is possible, though uncommon, to have abnormal thyroid function or thyroid antibodies with normal TSH.
Thyroid examination and tests for miscarriage
According to the American Society of Reproductive Medicine, endocrine disorders such as thyroid conditions may contribute to up to 20% of recurrent miscarriages.
If you already know that you have a thyroid disorder or a family history of thyroid disorders, your doctor will test your thyroid before or during pregnancy. If you have thyroid symptoms and have experienced miscarriage, you should definitely ask for a thyroid examination, and at least thyroid hormone (T4) and antibody tests.
The thyroid gland analysis includes a physical exam and blood tests to check for thyroid hormone levels and an ultrasound examination.
Thyroid exam
A thyroid exam is a physical examination that is not painful and lasts less than 5 minutes. Your doctor will stand behind you and put their hands on your neck to palpate your gland. After a few seconds, he or she might ask you to swallow and examine if there are enlargements or nodules present. No preparation for the exam is necessary. In addition, your doctor will also palpate the lymphatic nodes in the neck to evaluate their size, consistency, and whether they are painful or movable towards the skin or layers below.
Thyroid ultrasound
The thyroid ultrasound is a short procedure that lasts around 15 minutes. Your doctor will put an ultrasound probe with gel on your neck and look at the thyroid structures on the screen. The examination is not painful and doesn’t require any specific preparation. The ultrasound can identify thyroid nodules or tumors.
Thyroid blood tests
The thyroid blood draws are usually done first thing in the morning. If you are also testing for lipids and blood sugar first thing in the morning, you need to fast after dinner from the day before.
Hormones in the thyroid axis rise and fall following a specific pattern throughout the day 5. Sleep deprivation, jet lag, or taking blood samples later in the day can alter the TSH number even though your thyroid function is normal. To have an accurate number, go for a blood draw first thing in the morning after a good night of sleep. This may be especially important for the correct diagnosis and thyroid medication dosage.
Table: Changes in thyroid function during pregnancy for normal pregnancy and in women with thyroid diseases 6
| Maternal thyroid status | TSH | Free T4 (fT4) | Total T4 (tT4) | Free T3 (fT3) | Total T3 (tT3) | Free T3 index | T3* uptake |
| Normal thyroid function | Decrease | No change | Increase | Increase | Increase | No change | Decrease |
| Hypothyroidism | Increase | Decrease | Decrease | Decrease/ no change | Decrease/ no change | Decrease | Decrease |
| Hyperthyroidism | Decrease | Increase | Increase | Increase/ no change | Increase/ no change | Increase | Increase |
*T3 uptake is a measure of TBG level, which indicates the percentage of thyroid-binding globulin in blood samples.
Table: Trimester-specific Reference Ranges for Common Thyroid Tests 7
| Tests | Nonpregnant | First trimester | Second trimester | Third Trimester |
| TSH (mIU/L) | 0.3 – 4.3 | 0.1 – 2.5 | 0.2 – 3.0 | 0.3 – 3.0 |
| Free T4 (ng/dL) | 0.8 – 1.7 | 0.8 – 1.2 | 0.6 – 1.0 | 0.5 – 0.8 |
| Total T4 (mcg/dL) | 5.4 – 11.7 | 6.5 – 10.1 | 7.5 – 10.3 | 6.3 – 9.7 |
| Free T3 (pg/mL) | 2.4 – 4.2 | 4.1 – 4.4 | 4.0 – 4.2 | Not reported |
| Total T3 (ng/dL) | 77. 135 | 97 – 149 | 117 – 169 | 123 – 162 |
| TBG (mg/dL) | 1.3 – 3.0 | 1.8 – 3.2 | 2.8 – 4.0 | 2.6 – 4.2 |
| TgAb (IU/ml) 8 | 5 – 100 | n/a | n/a | n/a |
| TPOAb (IU/ml) 9 | 1 – 16 | n/a | n/a | n/a |
| TSHRAb 10 | 0 – 0.55 | |||
| rT3 11 | 250 pg/mL or 10 – 24 ng/dL |
1) Thyroid-stimulating hormone (TSH)
High TSH is a typical screening test for primary (originating in the thyroid gland) hypothyroidism. Previously, the TSH cutoff was 4.5 – 5.5 mIU/L, and some labs may still use this reference range. However, in 2012, the American Thyroid Association indicated that 2.5 mIU/L should be the cutoff for preconception general health and best pregnancy outcomes.
Women with TSH between 2.5 and 5.0 mIU/L are at an increased risk of first-trimester miscarriage 12. Using the cutoff at 2.5 mIU/L, there is no evidence of thyroid disease 13. In a large study, ~20% of women with recurrent pregnancy losses have TSH levels between 2.5 – 4.5 mIU/L 14. The current treatment guideline for thyroid disorders recommends titrating the medication until TSH is under 2.5 mIU/L 15. However, there is still limited evidence on whether starting levothyroxine when TSH is under 4.5 mIU/L is beneficial.
During pregnancy, natural TSH levels decline as human chorionic gonadotropin (HCG) acts like TSH, while total thyroid function increases. If you have pre-existing hypothyroidism, your doctor may increase your medication dose by 30% more 16. Also, it is important to check for TSH, T4, and thyroid antibodies every 4 – 6 weeks if you have diagnosed or suspected hypothyroidism.
2) T4 and fT4
Your doctor may test both TSH and T4 in case TSH alone may not reflect the full picture. It is possible, although less common, to have hypothyroidism with normal TSH. When TSH is normal but fT4 is low, it is called “isolated hypothyroxinemia.” It is controversial whether to treat low T4 alone during pregnancy, so your doctor may decide on a case by case basis 17.
3) T3 and fT3
Although T3 is the primary active hormone, it is rarely tested because T3 levels reflect the conversion of thyroid hormones rather than thyroid function itself. Your doctor is more likely to test T3 if they suspect hyperthyroidism than if they do hypothyroidism. T3 often increases before T4 in hyperthyroidism.
4) rT3
rT3 is the reverse mirror image of T3. Like T3, it is synthesized by removing an iodide from T4. However, rT3 blocks thyroid hormone receptors instead, resulting in overall reduced thyroid function.
Euthyroid sick syndrome or non-thyroidal illness are terms that are used to explain low thyroid function from other illnesses. People who suffer from the euthyroid sick syndrome, including 70% of patients hospitalized with non-thyroid conditions, often have low T3 and increased rT3 with normal T4 and TSH 18. In these cases, it is typically better to address the condition that reduced the T3 in the first place. Other causes of this syndrome include stress, infections, burns, traumas, metabolic disorders, kidney issues, and surgeries. There is no evidence linking euthyroid sick syndrome with miscarriage, but it is plausible.
5) Thyroxine-binding globulin
Thyroxine-binding globulin (TBG) is a protein produced in the liver. It binds to thyroid hormones outside the thyroid and helps transport them through the blood. It helps maintain a narrow range of active thyroid hormones 19. TBG levels may compensate for the increased or decreased output from the thyroid gland. TBG also increases when high estrogen increases 20.
6) Thyroid antibodies
Having thyroid antibodies is a disorder of the immune system rather than the thyroid itself. These antibodies may target proteins of the thyroid or proteins that affect thyroid hormone function.
Table: Different thyroid antibodies, their effects, and thyroid conditions in which they are found
| Protein attacked by antibodies | Antibody names and synonyms | Effects | Found in |
| Thyroglobulin (Tg) | Thyroglobulin antibodies (TgAb) | Nothing or thyroid inflammation and destruction | Hashimoto’s |
| Thyroperoxidase (TPO) | Thyroperoxidase antibodies (TPOAb) | Nothing or thyroid inflammation and destruction | Hashimoto’s |
| TSH receptor (TSHR or TR) | TSH receptor antibodies (TSHRAb or TRAb)Thyroid stimulating immunoglobulin (TSI) | May stimulate, block, or do nothing to TSH receptors, depending on the case. | Grave’s, Hashimoto’s, and Atrophic thyroiditis |
TPOAb is generally more problematic and more common in Hashimoto’s and postpartum thyroiditis. Some people with normal thyroid function have TgAb and TPOAb, whereas TSHRAb is only found in Grave’s and some Hashimoto’s patients 21.
Thyroid antibodies are naturally highest during the first trimester and decline throughout the pregnancy, but significantly increase again postpartum. Women with thyroid antibodies are at high risk of developing hypo or hyperthyroidism, especially postpartum. This is called postpartum thyroiditis.
5) Other lab markers
To diagnose thyroid disorders, your doctor may also take into account these other markers:
- High total cholesterol with high low-density lipoprotein (often called “bad cholesterol”) 22
- Elevated atherogenic (heart disease-causing) Lp(a) 23
- Increased creatine kinase 24
- Decreased heart rate
How thyroid hormones fluctuate during pregnancy
Pregnancy places a lot of demand on your thyroid glands, which may explain why thyroid disorders often contribute to pregnancy complications and miscarriage.
Your thyroid hormone function increases significantly during the first trimester and drops in later trimesters. The thyroid hormones control placental tissue development. In the first trimester, it also produces the hormones for both the mother and the fetus before the fetus can produce its own thyroid hormones. The thyroid glands may enlarge during this time. HCG works like TSH to stimulate the thyroid hormones both for the mother and the fetus. Later in the pregnancy, as the fetus develops its own thyroid, the mother’s thyroid function declines. The increased need for thyroid function and thyroid hormone production during pregnancy also explains the increased need for iodine during pregnancy 25.
Thyroxine-binding globulin (TBG), which transports thyroid hormones in your blood, also significantly increases during pregnancy. Levels typically peak by 16 weeks and remain high until delivery 26.
Conclusion
Pregnancies and miscarriages can change thyroid values or cause thyroid antibodies, so it is important to test every 4 – 6 weeks. You should also ask for your own copy and keep track of your thyroid labs. Also, the best levels for conception are different from the lab normal levels. In our Moving Forward Course, we teach you how to do this and include a Lab Tracker as a tool to make it easier for you.
Next Steps to Consider
- If you are experiencing infertility or miscarriage, make sure to have your thyroid levels tested, keeping in mind that levels can change over time, including post-pregnancy or miscarriage.
- If you do find your thyroid levels are off, work with a doctor or other health care professional to improve your levels for optimal fertility and to increase your chance of a healthy pregnancy.
- Stay hopeful! Women diagnosed with thyroid issues can go on to have a successful pregnancy.
- To learn more about all the different thyroid disorders that can cause miscarriage, see Part 2 of this 2-part series: Thyroid Disorder, Autoimmunity, and Miscarriage
References




0 Comments